Medical Dermatology
Melanoma in Dallas
- Home
- Medical Dermatology
- Skin Cancer
- Melanoma in Dallas
Learn How to Prevent, Diagnose, and Treat This Deadliest Form of Skin Cancer
In the world of skin health, one of the most-concerning diagnoses a dermatologist can make is melanoma. Dallas-area women and men should know that though melanoma is less common than basal cell or squamous cell carcinoma, it can be deadly, especially if a suspicious lesion is left unchecked or untreated. Unlike other types of skin cancer, melanoma can both spread outward on the surface of the skin and dive down into deeper tissue layers, as well as metastasize to other organs in otherwise healthy individuals.
Melanoma can affect people of ages, races and ethnic backgrounds. No one is exempt. Originally thought to be like other skin cancers, induced by sun exposure over time, melanoma is not caused solely from UV light exposure. As with any type of malignancy, it is important to teach patients with melanoma about sun protection and skin health, but in the list of causes for melanoma, the top factor is genetics. If there is a family history of melanoma, or of pancreatic cancer, it is important to have regular full body skin examinations performed by a dermatologist.
Medical Dermatology
Contact us online about setting up an appointment or call (214) 373-7546. Find out more about what to do about melanoma in the Dallas area today.
When a melanoma forms, it arises from an aberrant cellular overgrowth in the population of cells that normally exist in the skin to protect us from UV damage called melanocytes. For every 15 or so keratinocytes, or skin cells, we have approximately one melanocyte, which creates the pigment that gives our skin its background color, as well as to protect the DNA within those adjacent keratinocytes by sliding over it like a retractable awning when the skin cells are exposed to light. This DNA coverage is why lighter skin tans or darkens when exposed to light.
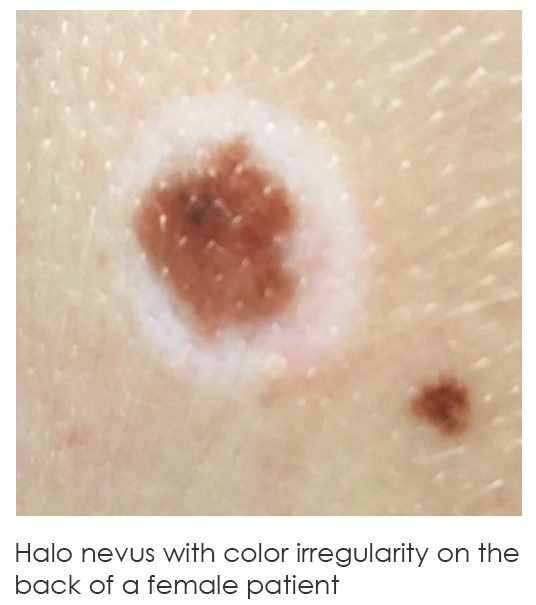
A large population of melanocytes in one small area is known as a mole or nevus. It was once thought that melanomas may only arise within a mole, but we now know this is not true. Melanoma may also arise spontaneously.
The earlier melanoma is caught, the better the prognosis for a normal life span. If melanoma is left untreated, it can progress and metastasize, causing early death. Thus, it is very important for all patients, young or old, to know the signs of abnormal moles and melanoma, so that a dermatologist can be consulted immediately if there is cause for concern.
The simple way to remember the warning signs for possible melanoma are to use the ABC guidelines:
ASYMMETRY
If a lesion were to be split down the middle and flipped onto its side, would both sides mirror one another? If the answer is no, you have asymmetry, and this could be a warning sign for the presence of melanoma.

BORDER IRREGULARITY
Similar to the “asymmetry” guideline, irregularity in a lesion’s border indicates that there is no clear definition as to the edge where it meets non-affected skin. Where there appears to be protrusion or lobules of pigmentation at the borders, rather than a neat circle or oval appearance to the pigmentation, this indicates border irregularity and could be a warning sign as well.
COLOR
Variations in the color of a mole, such as multiple shades going from tan to medium brown to dark brown or even black, can indicate there is an irregularity in the melanocyte population, including melanoma. Sometimes, melanomas can even be shades of gray or blue. Additionally, melanomas are sometimes amelanotic, meaning there is a complete absence of pigment. Typically, though, these amelanotic melanomas present as a bleeding lesions that draw patients into the dermatology office.
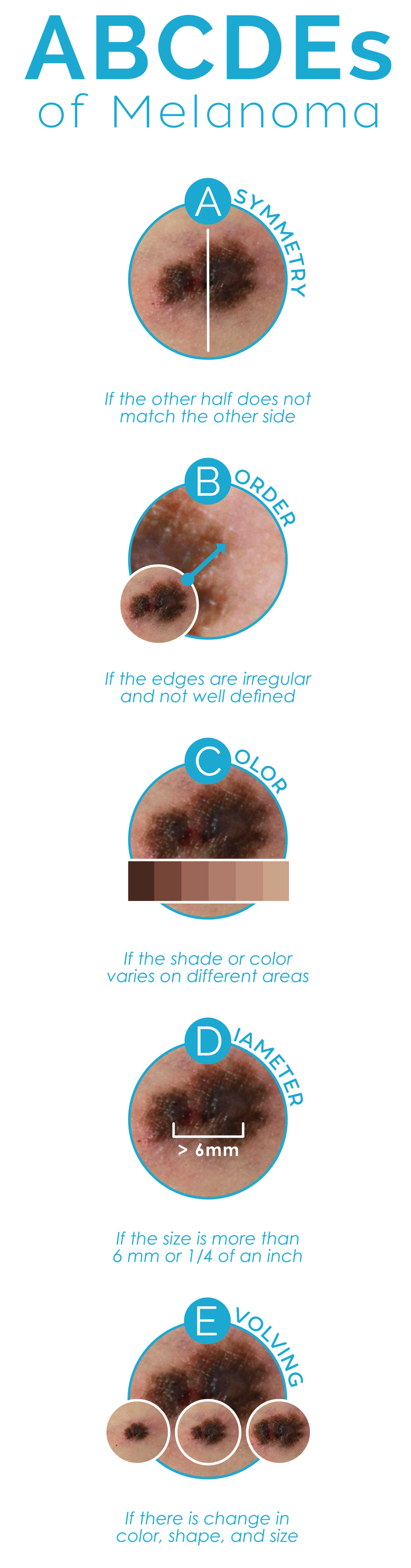
DIAMETER
Some moles are naturally larger than a pencil eraser, or greater than 6mm in size. In the case of a child, as the child’s skin grows, so does the size of the moles, however it is always a good idea to have a dermatologist check all moles, especially if they are larger than the diameter of a pencil eraser, as this could be a warning sign.
EVOLVING
This last guideline was also the most recently added, and it makes a lot of sense. If a mole or something similar on the skin is new or changing and evolving, it is important and necessary to have a dermatologist evaluate it for normalcy. Not all new lesions are malignant, but it is best to get any new or changing lesions checked.
The gold standard for proper diagnosis of an abnormal mole or melanoma is for the dermatologist to perform and fast and easy skin biopsy on the same day of the skin evaluation. This process begins with locally numbing the area using an injection of local anesthesia such as lidocaine, which acts in seconds. Next a surgical blade is used to remove the sample. Lastly, the specimen obtained is sent to a specialty pathologist known as a dermatopathologist, someone who is trained extensively in general as well as dermatology pathology. The report typically takes less than a week to return, and the patient is notified as to the results.
If a melanoma is diagnosed, depending on its depth—which is determined by the dermatopathologist upon review of the biopsy—the patient may be referred to a surgical oncologist, and possibly even a medical oncologist for a team-based approach to the treatment. The dermatologist is always an integral partner in continuing treatment and prevention as the full body skin examinations increase during the first year post-diagnosis, to every three months, and then to twice yearly thereafter. At no point in time will the frequency of dermatologic full body skin examinations decrease during a patient’s lifetime, as this is key to noting suspicious lesions as early as possible.
If diagnosed early, melanoma is very treatable, and patients can have a normal quality of life and little or no impact on their lifespan.